Key Takeaways
- Social isolation – defined as the objective lack of (or limited) social contact with others – has reached historic heights in every age group.
- As far back as we can measure, average social isolation has consistently risen with age.
- However, recent trends – including effects stemming from the COVID-19 pandemic – indicate an especially sharp rise in social isolation among younger age groups.
- Combatting the threat of social isolation will require outreach efforts and investments to increase opportunities for social connection in every generation.
Social isolation – defined as the objective lack of (or limited) social contact with others1 – has long been viewed as a pressing concern for older adults. Decades of data show that social isolation rises steadily with age; however, a deep dive into recent trends reveals troubling developments in younger age groups, including significant increases in isolation before and during the COVID-19 pandemic. These findings demonstrate that social isolation is an increasingly universal challenge and represent a call to action for initiatives which promote increased social contact for members of every generation.
An extensive body of research on social isolation exists; however, approaches to measuring isolation and related concepts (e.g., loneliness) vary widely.2 In this article, we use data from the American Time Use Survey (ATUS) to examine the average amount of time spent alone over the course of a day during 2010-2021.3 This is a common metric for quantifying social isolation in populations, as it provides a nationally representative, objective measure of interpersonal contact which can be tracked over time.
In 2010, average social isolation was lowest among those ages 15-24, who spent 28 percent of their time alone, on average. This percentage rose steadily with age, including particularly significant increases beyond age 44. Individuals age 65-plus were far more isolated than any other age group, with the average person in this range spending 53.6 percent of their time alone. As staggering as this latter value is, social isolation in the 65-plus population rose very little between 2010 and 2019. In contrast, average social isolation rose markedly among younger age groups during the same period, including a seven percentage-point increase for people ages 15-24.
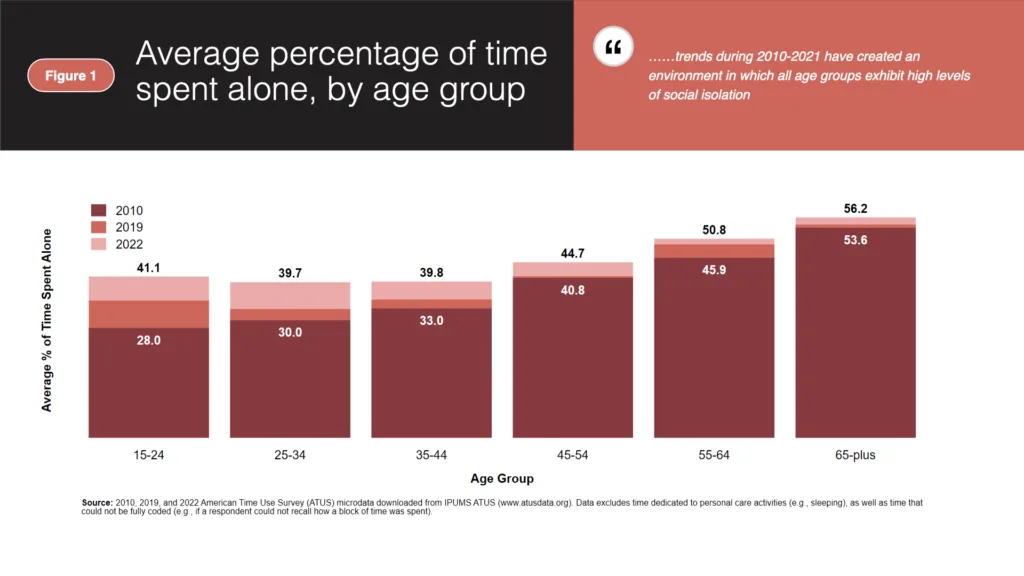
The most surprising finding shown above relates to growth in social isolation after 2019. Contrary to the common narrative that older adults were more susceptible to increased isolation during the pandemic, we find that the average percentage of time spent alone increased the most for people under age 35 between 2019 and 2021. In contrast, the average person over age 55 experienced a comparatively mild increase in social isolation over the same period, although this likely reflects the fact that social isolation was already very high in this group prior to the COVID-19 pandemic and consequently had limited capacity for additional growth. In any event, prevailing trends during 2010-2021 have created an environment in which all age groups exhibit high levels of social isolation.
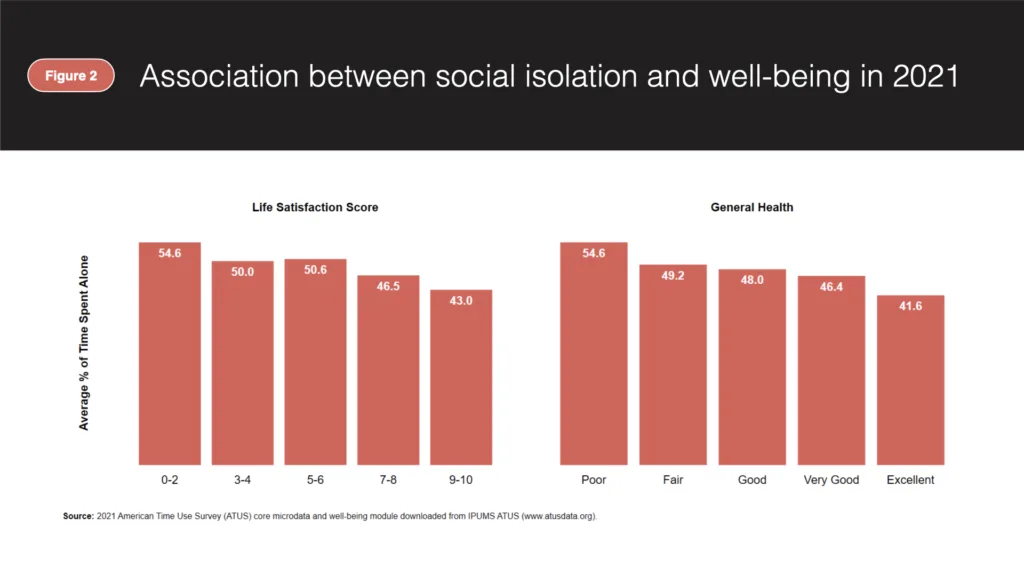
A lack of in-person interaction is not necessarily a negative outcome for any specific individual, and there is no established threshold for how much time a person should spend alone. Similarly, one’s level of isolation says nothing about the quality or their social interactions, and individuals experiencing little-to-no social isolation are not immune to problems such as loneliness. However, there is strong evidence that higher average social isolation is correlated with negative health and wellbeing outcomes in populations. For example, survey results from 2021 indicate that individuals who report greater social isolation also tend to have lower life satisfaction and poorer general health. In fact, the average person who reported having poor general health in 2021 spent 54.6 percent of their time alone, 13 percentage points greater than the average person who reported having excellent general health. Similarly, individuals reporting the highest level of life satisfaction are also the least isolated, on average.
For as far back as we can measure, people age 65-plus have faced higher average social isolation than their younger counterparts. However, recent trends show that the youngest age groups are increasingly at risk. These findings strongly agree with recent research, including a May 2023 advisory from the surgeon general, which characterizes isolation and loneliness as an epidemic in the United States. Combatting these trends will require widespread outreach efforts aimed at identifying isolation and increasing opportunities for social interaction at every age. AARP has been at the forefront of this field for years; for example, AARP Foundation’s “Connect 2 Affect” tool helps individuals assess their level of isolation and find resources in their area to improve social connectedness. Similarly, AARP’s Fun & Fulfillment initiative includes a range of programs designed to increase social engagement among older adults. AARP has also completed research identifying additional practical steps, such as the development of standardized screening tools for tracking social isolation in individuals (e.g., during annual wellness visits). In the wake of a devastating pandemic, efforts such as these recognize the diverse set of people experiencing high levels of isolation and offer solutions that promote greater social interaction at any age.
- This definition comes from Box 6.1 (pg.108) of Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System (https://doi.org/10.17226/25663). This book was produced by The National Academies of Sciences, Engineering, and Medicine and published by The National Academies Press in 2020.
↩︎ - Chapter 6 of Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System (https://doi.org/10.17226/25663) provides a useful review of approaches to measuring social isolation. The metrics discussed in this chapter vary widely in their subjectivity, as well as the underlying concept of social isolation used. The measure used in our analysis emphasizes the objective level of one’s social interaction; as such, it is consistent with the National Academies’ definition of social isolation and conceptually linked to measures such as the Berkman-Syme Social Network Index. ↩︎
- Our specific measure of social isolation is the fraction of one’s time spent alone during a 24-hour period, excluding time spent on “personal care activities,” which includes sleeping and personal activities like grooming. We also exclude time that is not fully coded in the data (e.g., time during which the respondent cannot recall if they were alone). For example, if an ATUS survey respondent spent eight hours sleeping and one hour on other personal care activities during their time diary day, then they would have 15 remaining hours that might be spent alone or with others. If this respondent spends six of those hours alone, then we record them as having spent 6/15 = 40 percent of their time alone. This metric is very similar to measures used in recent work by Pew Research, working papers such as Atalay (2022), as well as peer-reviewed academic studies such as Kannan and Veazie (2023).
↩︎

 "
"
